Africa pandemics: Collaboration and sharing resources will advance excellence
By Quarraisha Abdool Karim
Africa is plagued by many epidemics, from tuberculosis and HIV/Aids to malaria and wild polio. But the continent has also worked for decades to overcome these threats. The key to managing these deadly diseases is turning inward to existing expertise and finding locally driven solutions.
The recent Covid-19 pandemic has placed public health back in the global spotlight and served as a reminder that science is not undertaken in an ivory tower. Science shapes humanity because it takes place among us. Covid has also showcased that no epidemic takes place in isolation. Through collaboration, we can build on our knowledge to innovate ways to address health challenges that benefit all of humanity.
This is not a new idea, it is something we became all too familiar with during the Aids pandemic. Despair, pain and loss were rampant in the 1980s and early 1990s, at the beginning of South Africa’s HIV epidemic. White funeral tents mushroomed and multiplied every weekend in rural KwaZulu-Natal, signifying the growing toll the virus was taking.
Witnessing this helped catalyse me to undertake one of the earliest population-based studies that looked closely at this emerging health issue in South Africa. HIV prevalence was low at the time, with less than 1% of the population infected, but lurking in the data was a shocking revelation: young women (15 to 24 years old) were six times more likely to be infected compared with their male counterparts.
We knew something had to be done. That meant understanding what led to this striking disparity in risk. So, we began speaking to women from all sectors of society to try to get a better sense of what they were experiencing.
Local innovation
We learned that power dynamics in relationships and sex were disrupting disease prevention. Women did not have the ability to protect themselves because of the limited options available to them, such as condoms, which placed the responsibility of reducing risk in the hands of men. Meanwhile, cases continued to surge at an alarming rate, doubling every year in the general population.
Existing methods to prevent HIV infection were not going to cut it. Approaches designed in the Global North were never going to account fully for the needs of women in Africa. New solutions had to be brought forward.
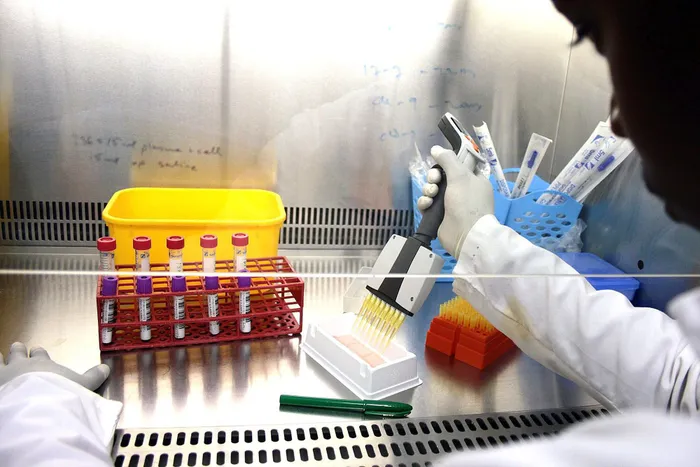
One way we sought to empower women was through a gel that contained tenofovir, an antiretroviral medication. This innovative approach, shown in the Centre for the Aids Programme of Research in South Africa (Caprisa) 004 trial, enabled HIV-negative women to protect themselves against the virus. The VinFuture Prize recently recognised Caprisa’s research on pre-exposure prophylaxis (PrEP) as a life-saving innovation from the Global South.
Today, tenofovir is taken daily as a pill for HIV prevention. The World Health Organization has adopted it as a key prevention option for women and men and it hasn’t stopped there. A range of new antiretroviral drugs and long-acting formulations, delivered as injections and implants, are being evaluated to expand prevention choices.
Aids is no longer a fatal condition, instead it is chronic yet manageable. But we still see too many deaths and new HIV infections, particularly in marginalised populations. Two-thirds of those with HIV and Aids live in sub-Saharan Africa and the region accounts for 60% of all new infections.
Lessons from the past
As we turn our focus towards other pandemics such as Covid, we cannot afford to lose the gains made in HIV. It is a trap we fell into before, when early HIV work overshadowed tuberculosis efforts, and it is not one we can afford to be caught in again.
Even now, Covid continues to draw on lessons from the decades of work that have been poured into our HIV and Aids response. This includes leveraging existing testing tools to detect the coronavirus, utilising clinical trial infrastructure to expedite vaccine development, calling on community engagement processes to educate the public and relying on scientific expertise to guide governments in their response.
The Aids pandemic taught us that scientists, policymakers and social organisations cannot work in a vacuum. There must be a unity of purpose that galvanises the support of global leaders in governments and funding agencies across the world.
Africa has the scientific leadership and intellectual capital to develop new technologies and interventions. This is something we have shown time and time again. If there is a problem, then local research is surely the best path to finding a solution.
Pursuing this path of innovation requires funding that supports and promotes the growth and expertise of Africa’s scientists. Our interdependency and shared vulnerability underscore the importance of collaboration and resource-sharing, globally and regionally, that must be used for the benefit of humanity. There is no time for complacency. We must ensure that solutions are tailored by local research to best benefit those in need.
Quarraisha Abdool Karim is an infectious diseases epidemiologist and associate scientific director of Caprisa. She was a 2021 laureate of the VinFuture Prize, in the Innovators From Developing Countries category.
The article was originally published in The New Frame.
Related Topics: